I am a planner and an interior designer. I have shaped my professional career around my passion for both and feel very strongly that they are inherent skills to one another. I do not differentiated between the two when someone asks me what I do. Often times people refer to me as an architect because I’m doing planning. But that is not the case. I, along with many professional designers, have a wide range of talents in spatial design and 3 dimension problem solving.
Over the past 20+ years since I earned my degree, understanding and integration in architecture has grown tremendously but misconceptions and lost opportunities still persist. More often than not a designer is brought on near the end of a project to layer in the color and finishes or furniture layouts and not integrated in the whole design process. The designer misses the crucial opportunities to contribute to the fit-out team and document the design elements throughout the phases.
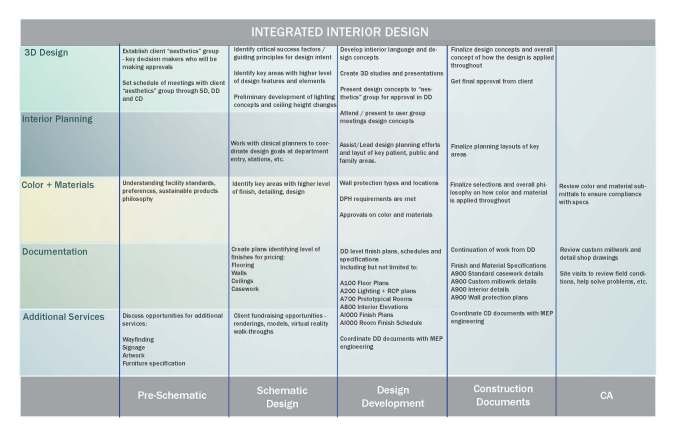
What does it mean for projects to have fully integrated interior design? How do you take a 2 dimensional plan and turn it into a beautifully designed and well-coordinated space that meets the clients expectations? Below is a chart illustrating key components a designer is responsible for | assisting on throughout all phases of the project with the main focus on interior design.